Is NIPT testing covered by insurance? This is a crucial question for expectant parents facing the cost of prenatal screenings. Insurance coverage for NIPT varies widely depending on the specific plan and individual circumstances. We’ll explore the nuances of insurance policies, the NIPT procedure itself, and the factors influencing coverage decisions.
Understanding the process of NIPT testing and how insurance companies assess its necessity is key to navigating the financial aspects of this important prenatal test. We’ll examine different types of insurance plans, potential costs, and the steps involved in securing coverage.
Insurance Coverage Overview
Insurance coverage for medical procedures, including non-invasive prenatal testing (NIPT), varies significantly depending on the specific plan and the circumstances. Understanding these nuances is crucial for patients to anticipate potential costs and make informed decisions. Insurance companies play a critical role in determining the extent of coverage for medical expenses. Different types of insurance plans offer varying levels of coverage, and patients must carefully review their policy documents to understand the specifics.
Insurance Plan Types
Different types of insurance plans, ranging from employer-sponsored health plans to individual policies, have different coverage policies. Understanding these distinctions is vital for navigating the complexities of medical costs. Employer-sponsored plans are often more comprehensive, but individual policies may offer flexibility in terms of choosing providers and procedures.
Role of Insurance Companies in Medical Expense Coverage
Insurance companies act as intermediaries, determining the extent of coverage for medical expenses. Their decisions are based on factors such as the specific procedure, the provider’s credentials, and the plan’s stipulations. A thorough understanding of the insurance company’s role empowers patients to advocate for their needs and understand their financial obligations.
Coverage Policies for Medical Procedures
Insurance coverage for medical procedures is not uniform across all plans. A comparison of coverage policies is presented in the table below. This data serves as a general guideline, and individual policies may vary.
| Insurance Plan Type | Coverage for NIPT | Copay/Deductible | Limitations/Exclusions |
|---|---|---|---|
| Health Insurance (Employer-Sponsored) | Generally covered, subject to plan specifics. May require pre-authorization. | Typically a copay and/or deductible, as Artikeld in the policy. | Certain providers may not be in-network. Specific tests or provider choices may be excluded. |
| Health Insurance (Individual) | May vary widely. Some plans cover NIPT fully, others partially, or not at all. | Copay and/or deductible dependent on the plan and the specific provider. | Out-of-network providers may have limited or no coverage. Coverage may depend on the type of NIPT test. |
| Individual Insurance (Short-Term/Limited-Term) | Often excludes or limits coverage for preventative or elective procedures like NIPT. | High copays and/or deductibles are common. | Coverage is often very limited and may not cover NIPT. Pre-authorization is almost certain. |
Factors Influencing Insurance Coverage Decisions, Is nipt testing covered by insurance
Several factors influence insurance coverage decisions for NIPT, including the specific test type, the provider’s credentials, and the patient’s location. Insurance companies prioritize cost-effectiveness and may exclude or limit coverage based on these factors. Furthermore, pre-authorization may be required before the procedure is covered.
NIPT Procedure and Costs
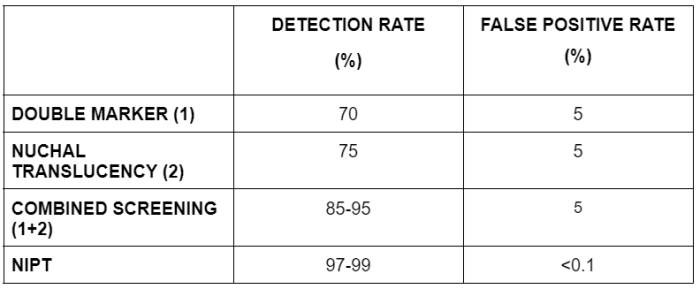
Non-invasive prenatal testing (NIPT) offers a significant advancement in prenatal care, enabling expectant parents to gain insights into their baby’s genetic makeup early in pregnancy. This method avoids the need for invasive procedures like amniocentesis, significantly reducing risks to the mother and fetus. Understanding the process and associated costs is crucial for informed decision-making.
NIPT Procedure Overview
NIPT involves extracting fetal DNA from maternal blood. This circulating fetal DNA (cffDNA) contains genetic information that mirrors the fetus’s genetic makeup. Specialized laboratory procedures analyze this DNA for chromosomal abnormalities, such as Down syndrome, Edwards syndrome, and Patau syndrome. The process typically begins with a blood draw from the expectant mother. The sample is then processed in a laboratory setting, using advanced genetic testing technologies.
Results are typically available within a few weeks.
Rationale and Implications of NIPT
NIPT’s primary rationale is to detect chromosomal abnormalities early in pregnancy, enabling timely interventions and support for parents facing such situations. Early detection allows for more informed decisions about prenatal care, potential interventions, and future planning. Furthermore, NIPT can reduce anxiety and uncertainty surrounding pregnancy, facilitating proactive management of potential complications. The implications of NIPT extend beyond immediate pregnancy concerns; it can offer peace of mind and empower families to prepare for the future.
Costs Associated with NIPT
NIPT testing costs vary significantly depending on several factors. Laboratory fees, physician fees, and any related expenses contribute to the overall cost. Expectant parents should carefully research and compare pricing from different providers. Transparency regarding pricing and associated expenses is vital.
Factors Influencing NIPT Testing Costs
| Factor | Explanation | Impact on Cost |
|---|---|---|
| Provider | Different laboratories and healthcare providers may have varying pricing structures due to operational costs, overhead, and technology investments. Independent labs, hospital-based labs, and specialized genetic testing centers often have different cost structures. | Can vary significantly, potentially resulting in substantial price differences between providers. |
| Insurance Plan | Insurance coverage for NIPT varies considerably across different plans. Some plans may cover the entire cost, while others may only cover a portion or none at all. The specific terms and conditions of the insurance policy play a critical role in determining the out-of-pocket expense. | Insurance coverage directly impacts the out-of-pocket cost for the patient. Lack of coverage can result in significant expenses. |
| Complexity of Testing | Advanced testing options, such as multiple marker screens or additional genetic panel analysis, often increase the cost. The complexity of the test, including the specific markers or genes being screened, can influence the cost. | More complex tests usually result in higher costs. |
| Geographic Location | The cost of healthcare services can differ across geographic regions due to variations in the cost of living and operational expenses. | Location-specific variations in healthcare costs can affect the overall price of NIPT. |
Insurance Coverage for NIPT: Is Nipt Testing Covered By Insurance
Insurance coverage for non-invasive prenatal testing (NIPT) varies significantly across insurance providers and individual policies. Understanding the factors that influence coverage is crucial for expectant parents seeking to utilize this technology. Coverage decisions are often complex and may involve negotiations between the patient, their insurance provider, and the healthcare provider.
Factors Influencing NIPT Coverage
Insurance companies typically consider several factors when determining NIPT coverage. These factors include the specific circumstances of the patient, the type of NIPT test, and the insurance plan’s provisions. The clinical necessity of the test is paramount. Providers often require a physician’s recommendation justifying the test’s medical necessity. This is a key determinant.
Assessing Medical Necessity for NIPT
Insurance companies evaluate the necessity of NIPT by considering various factors. These factors include the patient’s age, family history, and any existing conditions. Specific risk factors, such as advanced maternal age or previous pregnancy complications, are crucial determinants. A physician’s assessment of the risk of specific genetic conditions and the potential benefits of early detection is essential in this evaluation.
Insurance providers often review the patient’s medical records to assess the clinical justification for the test. A thorough medical history and appropriate risk assessment are critical in the approval process.
Pre-authorization and Prior Approval
Pre-authorization and prior approval are critical steps in obtaining NIPT coverage. These processes involve notifying the insurance company in advance of the procedure. Insurance companies require confirmation that the test is medically necessary and aligns with their coverage guidelines. This step ensures the insurance company will cover the cost of the procedure. Failure to adhere to pre-authorization procedures may result in denial of coverage.
Steps in Obtaining NIPT Coverage
Obtaining NIPT coverage involves several key steps. First, the patient’s healthcare provider must submit a pre-authorization request to the insurance company. This request must include detailed information justifying the medical necessity of the test. The insurance company reviews the request and provides a response. If the request is approved, the patient can proceed with the NIPT testing.
If denied, the patient should appeal the decision. Appeals should clearly state the medical reasoning and support the request.
Insurance Coverage Scenarios for NIPT
Insurance coverage for NIPT can vary widely based on individual policies and circumstances. In some cases, insurance companies may fully cover the cost of NIPT testing. In other instances, partial coverage may be provided, or the test may be deemed entirely not covered. The specific circumstances of each case, including the patient’s medical history, the risk factors involved, and the specific insurance plan, determine the coverage outcome.
Figuring out if your insurance covers NIPT testing can be a real pain. It really depends on your specific plan, but you might want to check with your provider first. Luckily, if you’re in the mood for a tasty treat, you can always grab a slice at pizza and pasta factory port monmouth. They’ve got some seriously good options, but don’t let that distract you from your important health decisions.
Ultimately, contacting your insurance company directly is the best way to get a definite answer about NIPT coverage.
For example, a patient with a strong family history of a specific genetic disorder and a high-risk pregnancy is more likely to have NIPT covered than a patient with no such history. A comprehensive understanding of the specific insurance policy and medical necessity is crucial for securing coverage.
Variations in Coverage Across Plans
Insurance coverage for non-invasive prenatal testing (NIPT) varies significantly across different regions and insurance plans. This variability stems from the differing healthcare systems and reimbursement policies in place. Understanding these nuances is crucial for prospective parents seeking NIPT, as it impacts financial planning and access to this important diagnostic tool.NIPT coverage often depends on the specific type of insurance plan, including the plan’s network, in-network providers, and specific limitations regarding the procedure.
Factors like the plan’s formulary, which lists covered medications and procedures, significantly influence the degree of NIPT coverage. Furthermore, regional differences in healthcare regulations and reimbursement guidelines further complicate the landscape of NIPT coverage.
Regional Variations in NIPT Coverage
Geographical differences in healthcare systems and regulations lead to considerable variations in NIPT coverage policies. For example, in some regions, NIPT is frequently covered by private insurance plans, whereas in others, coverage might be limited or even nonexistent. These variations often stem from factors such as differing healthcare priorities and economic considerations within specific regions.
Insurance Plan Type and NIPT Coverage
The type of insurance plan (e.g., HMO, PPO, POS) can significantly affect NIPT coverage. HMO plans often have more stringent requirements regarding in-network providers, which can limit access to NIPT if the selected provider is not part of the network. Conversely, PPO plans typically offer more flexibility in choosing providers, potentially leading to broader NIPT coverage options.
Examples of Varying Coverage Policies
Consider a hypothetical scenario where a family in the United States has two insurance plans with different coverage policies. Plan A, a PPO, may cover 80% of the NIPT cost, while Plan B, an HMO, might only cover 50% or even require a copay. These differences can lead to significant financial burdens for those with limited or no NIPT coverage.
Another example is in Canada, where NIPT coverage is more often integrated within provincial healthcare systems, potentially impacting the cost and access to the procedure for patients.
Typical NIPT Coverage Percentages Across Insurance Plans
| Insurance Plan Type | Coverage Percentage | Notes |
|---|---|---|
| PPO | 70-90% | Coverage typically higher; co-pays and deductibles may apply. |
| HMO | 50-75% | Coverage often lower; in-network providers are crucial. |
| POS | 60-85% | Coverage varies; in-network or out-of-network options are available. |
| Government-sponsored (e.g., Medicaid, CHIP) | Variable | Coverage depends on specific program guidelines and regional regulations. |
Note: Coverage percentages are approximate and may vary significantly depending on the specific insurance plan, the region, and the provider.
Appealing Coverage Decisions
Insurance companies sometimes deny coverage for non-invasive prenatal testing (NIPT). This decision can be frustrating and concerning for expectant parents. Understanding the appeal process and the potential reasons for denial is crucial for navigating this challenging situation. This section will detail the process for appealing a denial, highlight potential reasons for denial, and offer examples of successful appeals.
Figuring out if your insurance covers NIPT testing can be a real pain, but thankfully, there’s a wealth of info out there. Learning how to whip up a delicious Smoothie King Angel Food, like in this guide how to make smoothie king angel food , might not directly answer the question, but it’s a great way to unwind while you research your options for coverage.
Ultimately, checking your policy details is key to knowing if NIPT testing is covered.
Process for Appealing a Denial
Successfully appealing a denied NIPT claim requires meticulous documentation and a clear understanding of the insurance company’s policy. A crucial first step is to carefully review the denial letter. Note the specific reasons for the denial and any supporting documentation. Then, gather all relevant medical records, including the physician’s recommendation for the NIPT, and any pre-authorization forms or completed applications.
Contact the insurance company’s customer service department to request a copy of their policy regarding NIPT coverage. Once you have all the required documents, craft a compelling letter to the insurance company’s appeals department, reiterating your request for coverage. Include all supporting documentation, explaining the medical necessity and highlighting any relevant clauses in the policy that may support your case.
Be prepared to answer questions and to provide additional evidence to support your claim. Maintain meticulous records of all correspondence and interactions with the insurance company throughout the appeal process. Be prepared for follow-up correspondence and potential additional requests for information.
Reasons for Denial
Insurance companies may deny NIPT coverage citing various reasons. These reasons can include: the test not meeting the criteria for medical necessity, the test not being a covered benefit, the test being deemed experimental or investigational, or the test not being considered medically appropriate for the specific circumstances. In some cases, the insurance company may claim that the patient has other options for achieving the same results, which is an insufficient justification in the eyes of a healthcare professional.
A lack of pre-authorization or an incomplete application is another reason for denial. The denial may also be due to a misinterpretation of the policy or a procedural error on the part of the insurance company.
Examples of Successful Appeals
Successful appeals often involve a comprehensive understanding of the insurance company’s policy and a strong case for medical necessity. One successful appeal involved a patient with a family history of genetic disorders. The physician’s recommendation for NIPT was based on the increased risk of these disorders and the potential for earlier intervention. The appeal emphasized the benefits of early detection and the potential impact on the patient’s health outcomes.
Another successful appeal involved a patient with a history of a previous pregnancy with a serious fetal anomaly. The physician’s rationale for the NIPT emphasized the importance of preventing recurrence and the potential to improve patient outcomes. These cases demonstrate that a well-supported claim with compelling documentation can significantly increase the chances of success in appealing a denial.
Role of Patient Advocates
Patient advocates play a vital role in navigating the complexities of insurance appeals. These advocates can help patients understand their rights, gather necessary documentation, and effectively communicate with insurance companies. Advocates can also provide valuable support during the stressful and emotionally taxing process of appealing a denial. They are familiar with the procedures, policy interpretations, and strategies for successful appeals.
Their objective and unbiased perspective can be extremely valuable to patients who are facing a denial of NIPT coverage. Their expertise is often instrumental in ensuring that patients receive the appropriate medical care and support.
Factors Affecting NIPT Cost and Coverage
Insurance coverage for non-invasive prenatal testing (NIPT) is not uniform and varies significantly based on several factors. This variability stems from the complexities of medical necessity assessments, plan-specific guidelines, and the inherent differences in individual circumstances. Understanding these factors is crucial for both patients and healthcare providers to navigate the process effectively.Insurance companies meticulously assess the medical necessity of NIPT procedures.
Factors such as the patient’s risk profile, family history, and the presence of pre-existing conditions heavily influence these decisions. A higher risk pregnancy, determined by medical factors, often justifies coverage, while a low-risk pregnancy may not meet the criteria. This ultimately impacts the cost and coverage of the test.
Factors Influencing NIPT Cost
Numerous factors contribute to the cost of NIPT, directly impacting the likelihood of insurance coverage. These factors include the complexity of the genetic analysis, the specific testing panel offered, and the geographic location of the testing facility.
- Complexity of Genetic Analysis: NIPT tests vary in their complexity, depending on the specific genetic markers being analyzed. More comprehensive panels, targeting a wider range of chromosomal abnormalities, inherently command higher costs. This increase in cost often outweighs the benefit of additional testing for patients with a low risk profile, leading to potential limitations in insurance coverage.
- Specific Testing Panel: The scope of the NIPT panel directly affects its cost. Wider panels that screen for a greater number of genetic conditions typically carry a higher price tag. Insurance companies may be more likely to cover more extensive panels for higher-risk pregnancies, while more basic panels might be considered less necessary in lower-risk pregnancies.
- Geographic Location: Variations in the cost of healthcare services across different regions significantly impact the cost of NIPT. Factors like regional healthcare pricing and facility-specific costs can influence the total price of the test. This variance needs careful consideration when evaluating the potential insurance coverage.
Factors Influencing Insurance Coverage Decisions, Is nipt testing covered by insurance
Insurance companies consider several factors when determining NIPT coverage. These factors are designed to ensure the test is used appropriately and not unnecessarily.
- Patient’s Risk Profile: A patient’s risk profile is a critical determinant in insurance coverage decisions. Women with a higher risk of carrying a fetus with genetic abnormalities, due to factors such as advanced maternal age, previous pregnancy complications, or a family history of genetic disorders, are more likely to have their NIPT covered. Insurance coverage decisions are often influenced by the perceived clinical need for the test.
- Pre-existing Conditions: Pre-existing conditions, particularly those that could affect the pregnancy, can influence insurance coverage decisions. Insurance companies may be more inclined to cover NIPT for patients with known conditions that could potentially increase the risk of fetal abnormalities. This is to ensure appropriate use of the test based on clinical necessity.
- Plan-Specific Guidelines: Each insurance plan has its own set of guidelines for coverage of NIPT. These guidelines often specify the criteria for medical necessity, the types of tests covered, and the maximum reimbursement amounts. Understanding the specific policy is critical in determining the potential for coverage.
Circumstances Affecting NIPT Coverage Amount
Several circumstances can affect the amount of NIPT coverage provided by an insurance plan.
- Plan Type: Different insurance plan types have varying levels of coverage. For example, a comprehensive health plan might offer more extensive coverage for NIPT compared to a basic plan. The level of coverage often reflects the plan’s overall financial structure and benefits.
- Deductibles and Co-pays: Deductibles and co-pays are crucial factors in determining the out-of-pocket expenses for NIPT. These expenses can vary widely depending on the insurance plan, potentially affecting the financial burden on the patient. Knowing the plan’s specific stipulations is essential for accurate cost estimation.
- Negotiated Rates: Some insurance plans negotiate discounted rates with healthcare providers for NIPT, which can significantly reduce the out-of-pocket cost for patients. Negotiated rates reflect the contractual agreements between the plan and the providers, potentially leading to varying financial outcomes.
Potential Disparities in NIPT Coverage
Disparities in NIPT coverage based on individual circumstances can arise from differences in risk profiles, plan-specific guidelines, and the availability of negotiated rates.
- Risk Profile Variations: Patients with higher risk profiles are more likely to have their NIPT covered, while those with lower risk profiles may face greater financial burdens or limited coverage. Insurance coverage decisions are based on perceived clinical need, thus influencing the disparity in coverage.
- Plan-Specific Differences: Different insurance plans have varying coverage policies for NIPT, leading to potential disparities in coverage amounts. The patient must carefully review their plan documents to understand the specific terms and conditions. A detailed understanding of the plan’s specific stipulations is crucial for navigating the insurance process.
- Negotiated Rates and Financial Burden: Disparities can arise if the healthcare provider does not negotiate favorable rates with the insurance company. This could result in a higher out-of-pocket cost for the patient. Negotiated rates directly affect the financial burden on the patient.
Conclusive Thoughts
In conclusion, NIPT testing coverage is complex and influenced by numerous factors. Knowing your insurance plan’s specific policies, understanding the NIPT process, and being prepared to appeal decisions are essential for making informed choices. This guide provides a comprehensive overview to help you navigate this crucial aspect of prenatal care.
Questions Often Asked
Does my specific insurance plan cover NIPT?
Unfortunately, this can’t be answered without knowing your specific plan details. Contact your insurance provider directly for clarification on their NIPT coverage policy.
What factors influence the cost of NIPT testing?
Factors like the testing provider, your insurance plan, and any additional tests ordered can influence the cost of NIPT. Your provider can provide more details.
What if my insurance company denies coverage for NIPT?
You have the right to appeal the decision. Review the reasons for denial and gather supporting documentation to present a compelling case.
How long does the appeal process typically take?
Appeal timelines vary, but typically involve several steps and potentially take a few weeks to several months. Keep detailed records of all communication.
